(Pixabay)
As COVID-19 continues making its way through the United States, the virus’ case fatality rate seems to be flattening, and dropped to 3.0 percent Sept. 1.
Reporter Mitch Legan got together with a group of local experts including Indiana University epidemiologist Ana Bento, IU Health infectious disease Dr. Tom Hrisomalos and Graham McKeen, IU’s assistant director of public and environmental health, for a Zoom call to discuss what that means, why that is and what we’ve learned about the coronavirus.
This conversation has been edited for clarity and conciseness.
Mitch Legan: The [COVID-19] case fatality rate has been dropping since May, according to Our World in Data, and it seems to maybe be flattening out a bit. Can someone tell me, is that the case and why might that be?
Ana Bento: That measure is not so much a measure of the burden of infection in a population, but is also dependent on things like access to health[care] and the demographics of the individuals that are getting infected in certain regions. So it's a very difficult metric to use as a “Yes, we're doing great.” Or “No, we’re not doing so well.”
READ MORE: IU Epidemiologist Bento Named To WHO Panel On Reopening Schools
Dr. Tom Hrisomalos: What we've seen here locally, and some of this has been reflected nationally, is that the average age of our cases has declined. I think our largest group was in the 20 to 29 age group here just recently. And we know that age and coexisting medical conditions are a major risk factor for mortality. So that's part of it.
Another part of it is we've learned a lot in the last few months and we know how to treat [COVID-19] better. We have medications, both the antiviral drug remdesivir and the use of steroids in particular, which are known to impact recovery and to a certain extent, mortality. And so we're using those very readily right now, which we were not doing earlier on in the epidemic. So I think those two things also play a role.
Graham McKeen: The 20 to 29-year-old demographic is the highest demographic in the state right now at 18.6 [percent]. Well, in Monroe County, that's 35.7 [percent]. So I think that's a big piece of it. And those age groups are the ones most likely maybe not following all the guidelines and attributing some of this spread with gatherings and other activities. A lot of this age group is also an age group that are essential workers in the service industry, as well. So they're out there a lot more, and maybe therefore more exposed. So I think it's a combination of factors that plays into that, as well as increased testing.
ML: What is IU Health doing that has changed since the beginning of the pandemic?
TH: It appears that this virus occurs in sort of stages. The early stage of the illness – perhaps the first week or so – is due to viral replication: the illness is due to the virus itself. The latter stages of the illness, perhaps after 7 to 10 days and longer, it appears that a lot of the morbidity of the illness is due to the immune response against it. It's an immune-mediated issue.
And so, what we've appreciated is that early on, [is] we should be treating people with things that impact viral growth and replication. So that's an antiviral drug like remdesivir. We're trying to start that as soon as possible when people are admitted to the hospital and are hypoxic.
Later on, what we've found is that steroid medications – anti-inflammatory steroids and other anti-inflammatory drugs, which we're experimenting with – moderate the inflammatory components and may help prevent people from having respiratory failure and may thereby prevent deaths.
ML: President Trump had that interview with Jonathan Swan where they kind of went back and forth. President Trump was pointing to the piece of paper and he says, “No, look at our case fatality rate. It's great.” And Jonathan replied with saying, “Yeah, well, that looks pretty good. But look over here at deaths per 100,000 population.” So, can I get the difference between those two and how both might be useful in combating this disease?
AB: They're actually answering two different things. If we're looking at the deaths per 100,000 in a given population, we're looking at excess deaths. We have more or less a measure of yearly deaths or monthly deaths that are kind of like the baseline mortality of a given population, a given country, a given state. And that can be caused by many things, ranging from the flu, comorbidities, accidents. And so, what that measure is telling us and why the Axios journalist was so adamant about that is that now, presently, the contribution of COVID-related deaths is above what should be acceptable, given what we should be doing.
In terms of deaths per number of cases, it actually tells you something else. It just kind of tells you in comparison with how many cases we have of COVID, how many of these are progressing to disease, severe disease. And therefore, some of those will die.
[They’re] not saying the same thing. One number will look better than the other. Because we know that the infection burden in the U.S. is enormous. So [case fatality rate] will look like “Oh, barely anyone – it’s subsiding,” right? But it also doesn't tell you a measure of burden. And it doesn't tell you a measure of severity, right? It's just the tip of the iceberg. The other measure [deaths per 100,000] is far more sobering because we're now saying, because all the problems we have public health-wise, COVID is now the biggest contributor to deaths at this point.
GM: We base those numbers on what is laboratory confirmed, what we know. And so, is the true mortality rate of COVID-19 [3.0 percent] in the U.S.? No, it's not. So that's why we want to know what that true infection fatality rate is. And our colleagues up at IUPUI, when they did this really great – and they will continue to do stages of this great seroprevalence study in the state – they were able to estimate that when you factor in those 43 percent of asymptomatic patients and maybe some pre-symptomatic cases that might be out there that aren't detected or are tested, then you get down to [a case fatality rate of] maybe 0.6 or so.
Again, not super deadly, but definitely deadly enough to cause issues that we're seeing now. And so I think it's a little silly when people are like, “Oh, this has a 99.8 percent survivability rate or whatever and it's not a big deal.” It's like, clearly that's not the case. Again, when you factor in 330 million people in this nation, those numbers can get rather damaging.
ML: Ana, last time we talked, we were talking about data coming from Europe and Australia [on schools reopening]. It was limited, and you said that was your big problem with it. It seemed to kind of point that children might not be contracting or spreading [COVID-19]. Now we have kids back in school in the U.S. and there seems to be some data coming out that kids are, in fact, getting this and passing it on. So can you kind of speak to that?
AB: Serology studies [and] household transmission studies are indeed showing that young kids are, in fact, getting infected. And we're now at a stage to develop studies that are actually going to look at directionality of infection. So one of the things that we're very interested in, in any sort of infectious disease transmission, is what we call “Who infected whom?” It's not to point a finger at anyone but is to actually try and see where can we best implement a policy that will break that chain, right?
I really don't have much of an update on the answer that I gave you a few weeks ago. But I can tell you that yes, indeed, children are part of the transmission chain. Their absolute role in terms of how infectious they are and how susceptible there are still very much in the air. And to be honest, all of the age groups – we still don't have a clear measure of how susceptible they truly are in relation to other age groups and how infectious they really are.
ML: We've seen [the virus] kind of go from the coasts to the Midwest. And now in Bloomington, we've got a university here. As we've talked about before, we've invited tens of thousands of students to come back. Do we have concerns that Monroe County could become a hotspot?
AB: Yes. And I say this with a smile not trying to be psychopathic. Yes, because it's emphatic.
The university is not walled. Communities are porous, communities interact. And one of the things that is concerning, particularly, is that areas like Bloomington who are seemingly not as affected as other areas – the other side of the coin is that possibly means that most of the population is, in fact, naïve. What I mean by “naïve” is susceptible still. So now all of a sudden you have this wave of new individuals coming into the community and [they] might be infected or not.
And that means that all of a sudden you can have these little sparks in the population because individuals are susceptible.
So you have these situations where now these individuals might be infected [and] come into a population that is mostly naïve or at least partly naïve – naïve enough such that there's no herd immunity. So it is a problem. Definitely.
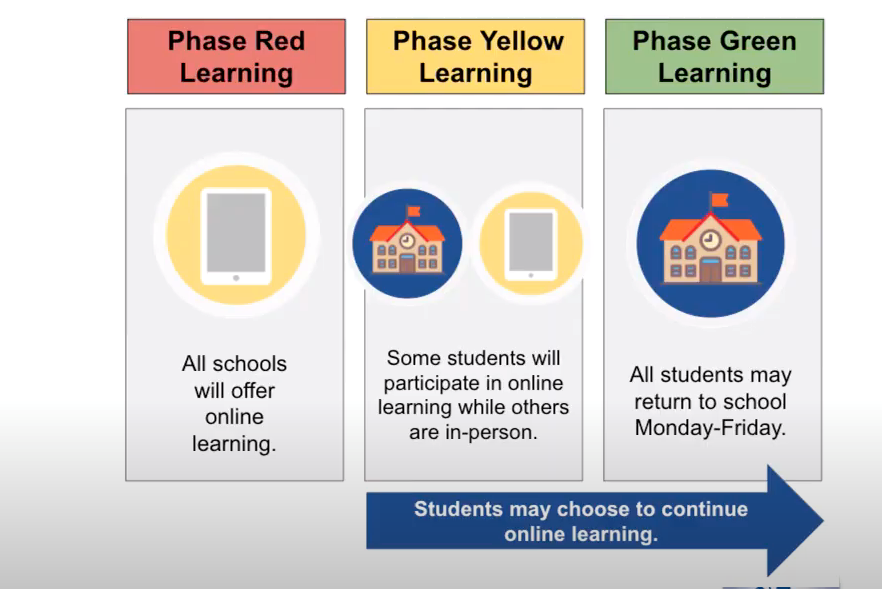
GM: I will say I don't think – as long as all of our students are here, I don't think in-person classes versus online makes really much of any difference in terms of transmissibility and numbers of outbreaks.
TH: I don't really have too much to add to that. I would agree that Indiana University has done just about as much as you can practically do, and I think that's great. The difficulty is that even when you do the most you can do, sometimes you can still fall short.
For the latest news and resources about COVID-19, bookmark our Coronavirus In Indiana page here.