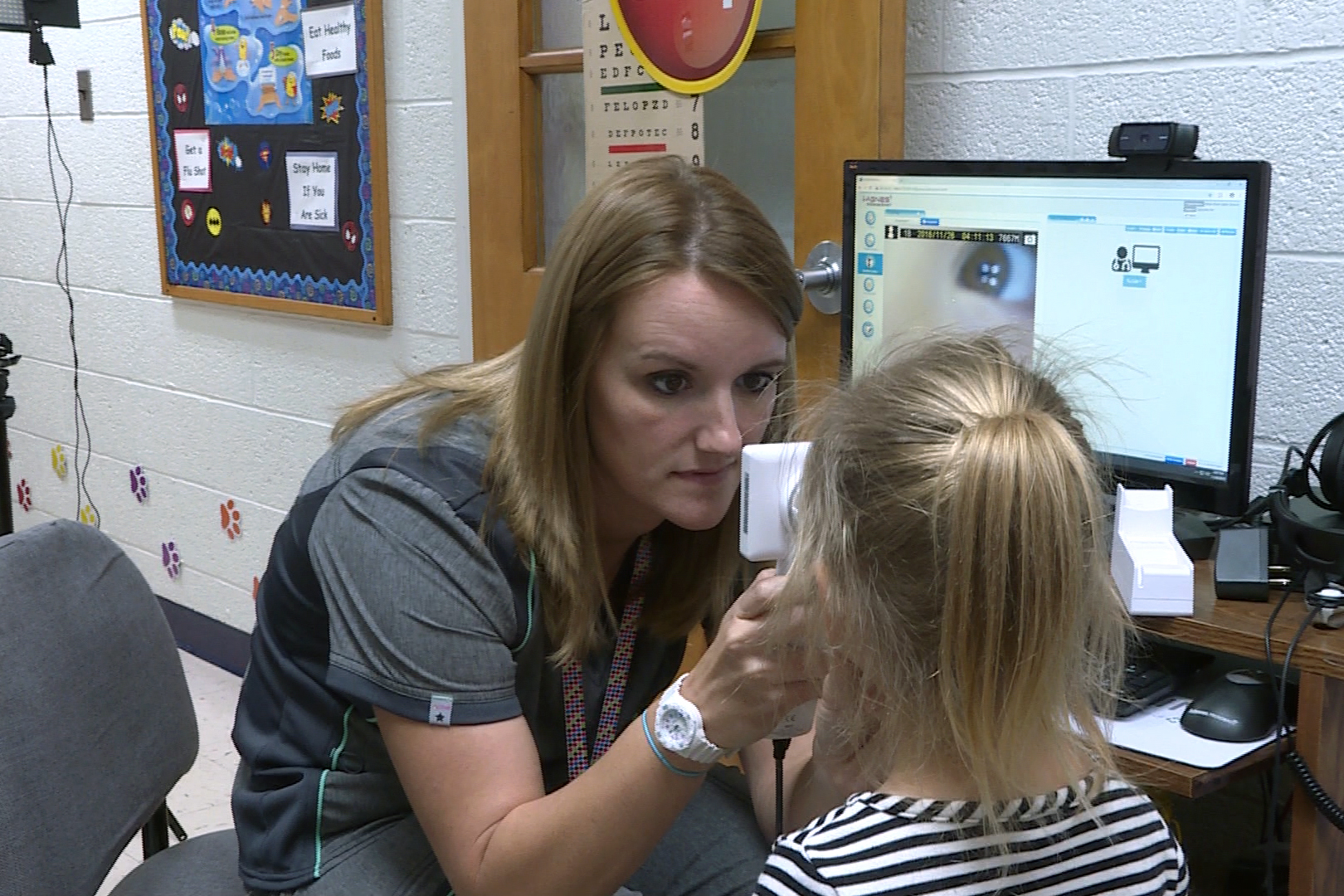
Many schools have moved their telehealth equipment, originally used by nursing staff, to rural emergency rooms and nursing homes. (Brock Turner, WFIU/WTIU)
COVID-19’s impact on medicine has been well documented, but the importance of telehealth has been augmented during the current pandemic.
Telemedicine has helped keep providers from bleeding more cash resulting from steep declines in patient visits.
HealthLinc, a community health clinic with 14 physical locations in northern Indiana sees around 14,000 patients every month, but only saw 8,000 in April.
Beth Wrobel, the company’s CEO, believes telemedicine — even if it’s unable to fully replace in-person care — is here to stay.
“If I have to take telehealth away from the patients and our providers there will be a mutiny,” she says. “Because it really does get people in and at the same time right now especially as we start to open up more visits, people are still afraid to come in.”
The pandemic has uprooted life as we know it. That’s also true for those who spend their careers in the telemedicine space.
Becky Sanders is the program director for the Upper Midwest Telehealth Resource Center. It’s a group that provides resources for providers trying to implement telehealth.
Sanders says the policy and reimbursement for telehealth has rapidly shifted in recent weeks.
“That is changing so rapidly,” she says. “There at the end of March, beginning of April, it was changing at an almost daily basis. So it’s finally starting to solidify and stabilize.”
Those changes have kept patients from traveling to their local doctor’s offices. For the first time, Medicare and Medicaid patients could be seen virtually from their homes. Sanders says calls have come from large insurance companies to primary care physicians.
“The emails and the phone calls have just gone through the roof,” she says. “It had been growing steadily over the past several years, but in the month of March we did more technical assistance than we had in the previous six months.”

One provider that has been forced to dive headfirst into telemedicine is HealthLinc. Wrobel is says adoption had to occur quickly.
“These were all things we had on our strategic plan for the next two to three years, and we did it in two weeks,” Wrobel says. HealthLinc continues to make adjustments to their procedures as needed.
For Wrobel, telehealth doesn’t replace services and care completed in-person, but rather supplements it. She says people have been hesitant to keep appointments, and believes increasing telehealth access will keep patients healthier.
As restrictions loosen and patients begin to venture out to their doctors’ offices, schools remain closed. One Indiana group that provides telehealth equipment to rural schools is working to redeploy that equipment to providers.
Kathleen Chelminiak is the project director for the Indiana Rural Schools Clinic Network which operates school-based telehealth services in 16 Indiana counties. She says her organization adapted to the pandemic too.
“Once COVID-19 hit, we quickly realized that schools were not going to be a place for children to receive care because of the mandated order that schools were to close," she says.
With schools closed, Chelminiak and her team quickly worked to try and match the equipment with a need. She says equipment from 15 schools is now being used in local ERs, nursing homes, and doctors’ offices.
“We’ve been able to bridge the gap of these rural areas needing the means to do telehealth visits in their practices and they didn’t have equipment otherwise," Chelminiak says.
And it’s that kind of collaboration and ingenuity that all believe will help push medicine and the standard of care forward — even in these trying times.
However, barriers to access remain. Many parts of Indiana lacks broadband internet coverage fast enough to support telehealth service. Despite legislative pushes, adoption is still lacking.
For the latest news and resources about COVID-19, bookmark our Coronavirus In Indiana page here.